Gastroshiza (Gastroschisis) – Symptoms, Diagnosis, and Treatment

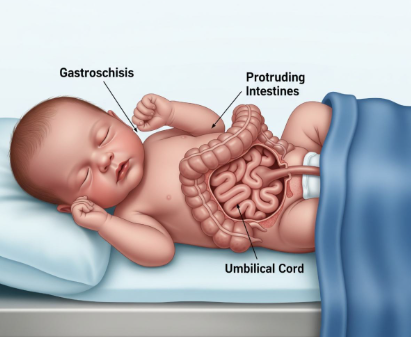
Gastroshiza, also known as gastroschisis, is a rare birth defect. In this condition, the baby is born with the intestines outside the body. The organs come through a small opening near the belly button. Unlike other abdominal wall defects, there is no protective sac covering the organs. This makes the intestines exposed to amniotic fluid during pregnancy.
The exposure can cause swelling and damage to the bowel. Gastroshiza is usually detected before birth, but in some cases, it becomes clear only at delivery. Doctors consider it a medical emergency because the exposed organs are vulnerable to infection and injury.
Causes and Risk Factors
The exact cause of gastroshiza remains unclear. Researchers believe it results from a combination of genetic and environmental factors. The abdominal wall forms in the early weeks of pregnancy. If the process does not complete correctly, a defect can occur. This defect allows the intestines to develop outside the body.
Possible Risk Factors
Several risk factors have been linked with gastroshiza. Young mothers under the age of 20 have a higher chance of having babies with this condition. Smoking, alcohol use, and recreational drug use during pregnancy may also increase the risk.
Some studies suggest that exposure to harmful chemicals or certain medications could play a role. Poor nutrition and low body mass index in mothers have also been noted as possible factors. However, no single cause has been proven, which makes prevention difficult.
How Gastroshiza Develops
During pregnancy, the abdominal wall normally closes by the tenth week. In gastroshiza, this closure does not happen correctly. A small opening remains next to the umbilical cord. Through this opening, the intestines come out into the amniotic fluid. Sometimes other organs, such as the stomach or liver, may also protrude.
The size of the defect can vary. In most cases, it is a small hole, usually on the right side of the belly button. Because the organs are directly exposed, they can swell and become thickened. This affects how well they function after birth.
Diagnosis of Gastroshiza
Prenatal Diagnosis
Gastroshiza is usually detected during routine pregnancy scans. An ultrasound performed around 18 to 20 weeks can show the intestines floating outside the body. Blood tests may also provide clues.
A higher level of alpha-fetoprotein (AFP) in the mother’s blood can suggest an abdominal wall defect. Doctors may use follow-up ultrasounds to monitor the baby’s growth and the condition of the exposed organs. Early detection allows specialists to plan delivery and treatment.
At Birth
If not detected during pregnancy, gastroshiza becomes obvious at delivery. The newborn will have intestines or other organs outside the body near the umbilical cord. Immediate medical care is needed to protect the organs and prevent infection. The baby is usually transferred quickly to a hospital with surgical facilities.
Complications Linked with Gastroshiza
Gastroshiza can lead to serious complications. The exposed bowel can become inflamed or twisted. This may block the passage of food. Some babies are born with too little intestine due to damage or underdevelopment.
This condition is called short bowel syndrome and it makes absorbing nutrients very difficult. Premature birth is also common in babies with gastroshiza. Feeding problems and growth delays may appear in the first weeks of life. Without treatment, gastroshiza is life-threatening because of the risk of infection, dehydration, and organ failure.
Treatment and Management
Immediate Care After Birth
When a baby with gastroshiza is born, doctors act quickly. The exposed intestines are covered with sterile dressings or placed in a protective plastic bag called a silo. This prevents the organs from drying out and reduces infection risk. The baby is given fluids through an IV, and a tube is inserted into the stomach to remove swallowed air and fluids. Body temperature and breathing are closely monitored until surgery.
Surgical Repair
Surgery is the only treatment for gastroshiza. If the opening is small and the organs are not badly swollen, doctors may perform a primary repair. This means pushing the organs back inside the abdomen and closing the hole in one operation. If the defect is large or the bowel is very swollen, a staged repair is done.
A silo is used to gradually return the intestines into the abdomen over several days. Once the organs are back inside, the opening is closed with stitches.
Recovery and Support
After surgery, babies often need intensive care. They may not be able to feed by mouth right away. Nutrition is given through IV until the intestines begin to function normally. Recovery can take weeks, especially if the baby was premature or if the bowel was damaged. Infections, feeding difficulties, and slow weight gain are possible problems during recovery. Doctors and nurses monitor the baby closely and provide support until normal feeding and growth are possible.
Prognosis and Long-Term Outlook
With modern medical care, the outlook for babies with gastroshiza has improved greatly. Survival rates are now higher than 90 percent in developed countries. Babies with simple gastroshiza, meaning only the intestines are affected, often recover well after surgery. Babies with complex gastroshiza, involving damage or loss of bowel, may face long-term challenges.
They can have ongoing digestive problems, need special diets, or require long-term nutrition through IV. Some children may also need further surgeries. Despite these challenges, many children with gastroshiza go on to live healthy lives with proper medical care and support.
Prevalence and Global Trends
Gastroshiza is rare but increasing worldwide. It affects about 2 to 5 out of every 10,000 live births. In the United States, about 1 in every 2,400 babies is born with this condition. Rates have been rising in many countries for reasons not fully understood. Younger mothers appear to be more affected by this trend. Researchers continue to study the causes and patterns to better understand why it is becoming more common.
Differences Between Gastroshiza and Omphalocele
It is important to distinguish gastroshiza from omphalocele. In omphalocele, the organs are covered by a thin protective sac. The defect is usually in the middle of the abdomen at the belly button. Omphalocele is often linked with other birth defects and genetic problems.
Gastroshiza, on the other hand, has no covering sac. The opening is usually small and slightly off-center, mostly to the right of the umbilical cord. Gastroshiza is less often associated with other birth defects. The treatment and outlook also differ between the two conditions.
Conclusion
Gastroshiza is a serious but treatable birth defect. It happens when the baby’s intestines develop outside the body through a hole near the belly button. The cause is not fully known, but young maternal age and lifestyle factors may raise the risk. Diagnosis is usually made before birth by ultrasound. Immediate care after delivery and surgical repair are needed to protect the baby’s life.
With proper treatment, most babies survive and grow into healthy children, although some may face long-term health challenges. Awareness, early detection, and skilled medical care remain the keys to managing gastroshiza effectively.
